| eeeeeeeeeeeeeeeeeeeeeeeeeeeeeeeeee222222222222222222222222222222222222222222222222222222222222222222222222 | |
|
APPLICATIONS OF LASERS IN DERMATOLOGY
|
|
|
|
Lasers have been used in dermatology for more than 20 years. The first lasers used were the Ruby and Argon lasers, and a great deal of experience has been obtained particularly with the latter. The Argon laser has been used predominantly in the treatment of cutaneous vascular lesions and the CO2 laser both as a cutting and ablating tool. Recently due to better understanding and modifications of the new lasers especially the computerized ones, lasers are considered an indispensable tool for the dermatologist. Different skin lesions were hardly to be treated and not efficiently before laser. Certain types of lasers such as C02 laser is of great help to the dermatologist and are considered as "working horse" in that field. Although different lasers are available now with different applications for skin resurfacing, pigment treatment, vascular and hair removal, yet the use of laser should be monitored for selected cases due to the higher, expensive cost of treatment besides other factors which may be not accepted by patients. Usually we are faced by many patients who are afraid from laser surgery due to their belief that laser will cause cancer. In spite that we try to convince them that laser is nothing but light and it is used in delicate branches as ophthalmology, yet others are still and will not be convinced. Meanwhile, Goldman, who first used a laser as a surgical tool warns "If you don't need a laser, don't use one."
A laser is a device that generates an intense beam of light. The term "LASER" denotes Light Amplification by Stimulated Emission of Radiation. Light is part of the spectrum of the electromagnetic radiation. Under certain conditions light exhibits the characteristics of a wave. All effects of light including laser light on skin begin with the absorption of electromagnetic radiation (EMR). EMR is an important form of energy that exhibits both wave and practical properties because the energy of light is carried through the photons. Whenever a photon is absorbed some movement or separation of charged matter occurs in the cells and the energy carried in the photon is invested in excitation of the charges . Excitation and absorption of the energy is the basic of photobiological effects and laser application in treatment . There are important data concerning light used in laser treatment . These include the following: The wavelength : is defined as the distance between the crests of each wave and that determines the functional properties of the laser energy. Electromagnetic radiation with long wavelengths, measured in meters, is commonly used for radio and television broadcasting. Wavelengths in the 0.4-0.7um range form the visible light of the spectrum. Ultraviolet rays, X-rays and gamma are forms of electromagnetic radiation with the wavelengths shorter than the visible light. Amplitude Is the height of the wave with the maximum displacement from the zero position . Frequency Is the number of waves passing in a given point per second and is expressed in cycles per second. The shorter the wavelength, the higher the frequency, and the higher is the energy. Velocity This is a constant and is equal to 186000 miles per second. Surgical lasers fall between the longest and the shortest wavelengths, in the infrared and visible as well as the ultraviolet portions of the electromagnetic spectrum. Several lasers are commonly used in medicine. The type of laser depends on the active medium used. These may be C02 as in the Carbon dioxide laser, Ruby, in ruby laser, copper as in copper vapor laser and special dyes as in dye lasers. The most commonly used medical lasers are, the carbon dioxide, ruby, argon, krypton, YAG and Excimer. The components of laser system are:
Energy: The capacity to do work and is usually calculated as power multiplied by time of laser light exposed on the skin surface. The unit of measurement is a joule. Power: is the rate of flow of energy. This is calculated as energy divided by the time of application. The unit of measurement is the watt. One watt equals one joule per second. Power density: is the rate of energy delivery per unit of target tissue area. This is expressed in watts per square centimeter. Power density is determined by the power divided by the surface area of the beam or the spot size. It should be noted that increase in the power output vaporizes tissues rapidly and reduction in the spot size will increase in the energy and accelerates more tissue interaction. Fluence: is the energy density and calculated as the total energy divided by the cross sectional area of the beam. It is expressed as joules per square centimeter. It is calculated as the laser power multiplied by time of exposure over an area of spot size in cm2. If the heat is deposited at a rate faster than the thermal relaxation time, there will be minimal conduction of heat to the surrounding structure. Spot size: Large spot size allows for smoother, more uniform vaporization of tissues. The spot size is controlled by focusing or defocusing of the lenses. Simply by moving the hand piece towards and near the skin decreases the spot size, or away from the target increases the spot size. The smaller the spot size the greater tendency to create uneven ridges, furrows and bleeding. Larger spot size causes decrease in peripheral thermal damage. Thermal relaxation time This is the time required for the heated tissues to loose some of its heat through diffusion. It is the time needed for adjacent tissue to cool during laser surgery. This is very important which has a direct relation to tissue destruction.
Laser light has three special qualities that distinguish, it from the conventional light source .
MODES OF ACTION OF LASER LIGHT
HUMAN SKIN AND LASER INTERACTION The nature of interaction of all laser light with biological tissue can be described in terms of: Reflection: There is always a degree of reflection of laser light from the epidermis. Transmission: The laser light is transmitted through tissues to their target. Scattering: This occurs after the laser light is transmitted and passing the epidermis to deeper tissues. Absorption: This occurs by the target tissue of the specific type of laser. Absorbed laser light may cause tissue coagulation or vaporization. Characteristically, laser light searches for its target such as pigment, hemoglobin or water. Tissue coagulation: is related to the thermal effect .The conversion of laser energy into heat causes coagulation, sealing or cautary with minimal necrosis occurs with temperature above 45 degree centigrade. Tissue vaporization: This occurs with temperature over 100 degree centigrade , particularly with rapid heat transfer from the laser light to the tissues. This will lead to boiling of cellular fluid and complete destruction of cellular protein and the cell itself. The fume of this vaporized tissue causes small particles which is about one micron . It is of prime importance to use special laser mask during skin resurfacing especially viral lesions such as warts where inhalation of these fumes containing the viral elements may cause serious complications .The laser mask should have special specification to filter particles less than one micron .
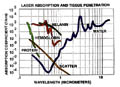
In laser tissue interaction, thermal coagulation causes cell necrosis, homeostasis, welding, ceiling of nerve endings and gross alteration of the extracellular matrix. Thermal coagulation is also a burn. Carbon dioxide lasers depend on evaporation of tissue water, which is the laser chromophore in these types of lasers. Other lasers target is the skin pigment such as pigmented cells, blood vessels and tattoo particles. Tissue damage depends mainly on the rate of energy deposition in the target. The fundamental processes govern all interactions of light with the tissue target are heat absorption or scattering. Heat is absorbed by the chromophore (melanin pigment. water, blood vessels) where each chromophore has a selective wavelength absorption .The absorption coefficient depends on the concentration of the chromophore present in the lazed tissue. Melanin: The first pigment that light encounters as it enters the skin. Melanin protects the skin from excessive sunlight, particularly the UV by absorption harmful wavelengths. This physical property of melanin makes it either aid or interferes with laser surgery depending on the type of lesion treated. Melanin occurs mainly in the epidermis and hair follicles absorb broadly across the optical spectrum. Hemoglobin: The iron containing pigment that makes blood red, blocks a large amount of light transmission into tissues. Hemoglobin has three absorption peaks: Blue (415nm), Green (540nm) and the Yellow (577nm). The optimum absorption is between 514-590 nm. Blood absorption is dominated by oxyhemoglobin and reduced hemoglobin absorption that exhibits strong bands in the UV, blue, green and yellow bands. The 577 nm (yellow) absorption band of oxyhemoglobin was chosen for targeting superficial micro vessels by selective photo thermolysis .The blue band (420 nm) or higher band 900nm penetrates more deep and can affect deeper target tissues. Scattering: Scattering is the third important factor in tissue interaction during laser therapy. The target, may absorb light entering the skin whether scattered or reflected. Most light entering the tissue is scattered by a very complete interaction with water. lipids and cellular membrane. Scattering is greater for short wavelengths of visible light. Scattered light is ultimately absorbed with the subsequent release of heat. Scattering is one mechanism whereby, heat is lost from the lesion being treated to be deposited in non-target tissue. Scattering is also the reason that the outline of bones cannot be seen when the hand is trans- illuminated. These three factors, melanin, hemoglobin and scattering are the basics in laser application in dermatology and cosmetology.
EFFECT OF LASER LIGHT ON THE SKIN LESIONS The epidermis is 100 um thick and is very susceptible to laser energy. It is almost universally damaged during laser surgery with visible light wavelengths unless adequately pre-cooled. The upper dermis is 400um thick and contains c'llary loops in the pegs supplied by the superficial arteriolar plexus. which is supplied from arteries in the lower dermis. The normal superficial plexus consists of 50um vessels and is a principle factor in skin coloration. The lower dermis is 400um consists of the supporting structures of the sweat glands, follicular structures and larger vessels. When laser is directed to skin, light may penetrate the skin surface, absorbed by the target tissue, reflected or scattered. There are three major factors, all-important in laser therapy, which keep tissue from being more transparent than it is. These are the targets for laser. Different lasers are principally depend on these factors, which are: the pigment melanin, hemoglobin and water. Pigmented lesions When treating a pigmented lesion, the light absorption characteristics of melanin are most important. Melanin is the target pigment or chromophore and is heated by absorption of the laser light to the point where the lesion is destroyed. The surgeon chooses a wavelength that is well absorbed by melanin. Generally a wavelength in the Blue/Green range is needed. Blue has higher absorption (but more scattering) than the green. Because of the increase of likelihood of scarring with the blue wavelengths, the typical choice for a pigmented lesion would be the green. Vascular lesions treatment Hemoglobin is the pigment target or chromophore for laser light. Any unwanted absorption in the skin by melanin would tend to heat non-targeted or non vascular tissue above or near the vascular lesion. Ideally the surgeon should be able to beam the light through the non vascular, melanin containing surface tissue without damage from their melanin absorption or scatter, and destroy vascular tissues beneath. He would choose a wavelength that is highly absorbed by hemoglobin and scatters minimally. Yellow wavelength : is the ideal and fits that most closely. Yellow light has minimal scatter and decreases absorption in melanin compared to green or blue. Longer wavelengths such as orange, red are not well absorbed by hemoglobin or melanin. Complications of laser surgery The complications which may be faced during laser surgery are: In vascular lesions treatment, scarring may occur if too much light energy is absorbed by he epidermis and perivascular dermis below the reticular layer of the skin. If the epidermis is damaged it can regenerate without scaring, while damage of the dermis may cause hypertrophic scarring. This is the worst complication when treating a vascular lesion as port wine stain with the use of Blue/Green wavelengths. especially in young children. Other complications besides hypertrophic scarring are hypopigmentation, hyper pigmentation and texture changes.
TYPES OF LASERS USED IN DERMATOLOGY Co2 laser is the most widely, precise tool used in dermatology, cosmetology and general surgery. The laser medium is mixture of carbon dioxide. nitrogen and helium gases, usually excited by direct current electricity . The C02 laser emits a continuous beam having a wavelength is 10600 nm , in the midinfrared portion of the electromagnetic spectrum. The beam of C02 laser is invisible and therefore a lowpower visible beam is used to provide an aiming dot for the surgeon to guide and direct the beam to the desired target . Laser energy passes through an articulated arm and focusing lens or through a hollow wave guided . The tissue target for this type of laser is water, where light is absorbed by biologic tissues causing destruction by rapidly heating and vaporization of the intercellular water. The strong absorption of the laser light by water causes tissue destruction "What you see during operation is what you get of the effect on human tissue ." The output power may exceed 100 watts in the continuous operation and 50 watts when using the pulsed operation . The factors affecting tissue destruction by laser is the power reaching the tissue , spot size and the thermal relaxation time ( which is the time between heating of tissues by the laser beam and the time of cooling of tissues). C O 2 lasers are now provided by computerized devices that make their use safer and much easier for the users . These computerized devices are programmed in a more simple way for use either for skin resurfacing, surgical cutting or simple ablation of the skin surface. The surgeon just uses the parameters according to the case he has to treat. The laser power and spot sizes are all adjusted automatically.
This is the first laser used by Dr. Goldman in 1965 for treatment of pigmented skin lesions and tattoos. Ruby laser (694 nm) of the Q-switched type can remove blue and black tattoo pigment. This type of laser can remove tattoos with minimal scarring and without anesthesia. Several sessions may be needed to remove pigmented lesions by the Qswitched Ruby laser. Different successful results depend also on the type of laser used.
Nd:YAG is another type of Q-switched laser with longer wavelength (1064 nm) and can be used to remove tattoos and pigmented skin lesions. The laser medium is neodymium-doped yttrium aluminum garnet crystal. This type is used in ophthalmology.
Several Metal lasers have been introduced recently which depend on a metal lazing medium heated above the boiling point to the gaseous state. Two different lights with two different wavelengths are emitted from this type of laser. The GREEN light at 511 nm is used for treatment of benign pigmentary lesions such as Cafe au lait spots , lentigo ,and benign dermal tumors . The YELLOW with a wavelength of 578nm is used for treatment of vascular lesions such as telengectasia.
The argon ion laser emits a beam of 488-514 nm is a blue green beam found in the visible portion of the electromagnetic spectrum . The excitation medium is the ionized argon gas in a sealed laser tube , which is excited by a direct current electrical discharge . This type is used in ophthalmology and in dermatology for treatment of haemangiomas .
The laser medium is holmium, emitting laser beam with a wavelength of (214nm )and excited by a flash lamp. This type is used for orthopedic treatment of torn meniscus, synovial disease , and articular degeneration .
These types emit beam within the ultraviolet portion of the spectrum from (193_351 nm ). These lasers are used in cardiovascular investigations to remove vascular plaques and in ophthalmology.
Laser emits an intense beam of electro-magnetic radiation that can easily cause irreversible damage to tissues, particularly ophthalmic tissue. therefore strict precautions should be taken into consideration when using lasers . Protection of the patient , the surgeon , the assistant is of prime importance.
USES OF LASERS IN DERMATOLOGY The uses of laser in dermatology have grown in the recent few years and based largely on better understanding and the modifications applied recently to different lasers. The C02 laser can be used to vaporize or to cut tissues. The important criteria in using C02 laser are the power output and the spot size. The spot size can be changed either by defocusing the beam, keeping the hand piece away from the treated area or by focusing the beam keeping it nearer to the area .Spot size of 2-5 mm is typically used for vaporization and the power output is decreased to get the best surgical results when doing vaporization . Uses of Co2 Laser Co2 laser can be used successfully to treat the following lesions: Skin resurfacing: removal acne scars, skin wrinkles, hypertrophic lesions of lichen planus, xanthelasma. seborrheic keratoses, psoriasis patches with excellent results by an experienced surgeon. Actinic cheilitis :C02 laser is the treatment of choice for treatment of actinic cheilitis.
Epidermal tumors: Warts treatment: of different sizes can be easily and effectively vaporized by C02 laser. It is recommended to use a magnifying lens during vaporization of warts. Warts typically bubble on evaporation . Precautions should be taken during vaporization of warts by using a special laser mask to filter wart particles during vaporization in order not to inhale the particles, which may cause infection to the surgeon. The surface of the wart is better shaved before laser vaporization to remove the dry hyperkeratotic surface, which requires much high energy because of its lower water content. Peri ungual warts can be vaporized and if the lesion is extending beneath and around the nail , the overlying nail can be evaporated to avoid nail avulsion. Vascular lesions: such as telengectasia, port-wine stains, angiomas. Epidermal pigmented lesions: Epidermal nevi, lentigines , ephelides, tattoo and pigmented labial macules. Tattoos: can be removed by vaporization the area with a bloodless fields. This method usually leaves scar. Other types of lasers such as Q-switched lasers are more efficient in removing tattoos without skin scarring . Benign dermal tumors: neurofibromas, myxoid cysts, and granuloma faciale. Actinic keratosis and squamous cell carcinoma. Debridement of burns. Control of bleeding. Cosmetic surgery: Rhinophyma, blepharoplasty, and mammoplasty. General Instructions. Patient Consent. The patient should sign a special form to agree about laser surgery and that he had information about that. The patient also understands that he has to abide with instruction of the surgeon and he accepts any complications, which may result after the surgery. The patient is instructed that there is an erythema resulting after the operation, which may extend for one month or more and he should keep away from direct exposure to sun light and use exactly the medications as prescribed. The patient should have information about the type of the skin lesion to be treated. The type of laser surgery to be applied. Result of Laser Surgery: It is very important that the surgeon should discuss to the patient be informed that "No human being by any device can return the treated area exactly the same to its previous condition." The surgeon will do his best and every unexpected situation may happen. The surgeon must not give too much hope for the patient, meanwhile he should be honest and wise in telling the whole story to his patient
ANESTHESIA FOR SKIN RESURFACING Local anesthesia
9. Local infiltration of the lesions by xylocaine.
SKIN CARE INSTUCTIONS AFTER LASER SURGERY The patient should be instructed to abide strictly with the following:
Postoperative measures. Apply polysporin ointment. We rise in our medical center combination of Pufexamac and Muperacin cream ( Droxaryl & Bactropan) that proved to have an excellent post-operative healing and minimizing er ythema arid hyper pigmentation . The resurfaced area can be covered by Vaseline or vigilion dressing. The dressing is left in site for 48 hours and then removed using only the medication without covering . Ice bags, cold milk compresses or Pufexamac cream (Parfenac, Droxaryl cream) can be applied several times a day to alleviate erythema and edema. Do not remove the Crusts. Emollients such as (Oileatum cream ) can be used to keep the skin moist. Washing can be permitted avoiding tissue papers for drying of the skin. Soft cotton towels can be used. Minimize irritation of the skin by gently drying without rubbing , just to press gently the cotton towel to the area. Avoid irritants to the resurfaced areas such as perfumes or strong soaps. Mild soaps can be used such as Alpha keri soap or white Dove soap. Avoid direct sun exposure: This may lead to hyperpigmentation especially in colored individuals.
Ablation: removal of tissue by vaporization. Beam: a ray of light. Divergence: increase in beam diameter with distance from the exit aperture of laser. Chromophore: optically active material in tissues that can act as an absorptive target for laser (melanin, hemoglobin water). Absorb: To take up matters or energy. Absorption coefficient: Ability of light to be absorbed. Active medium: The active material in the laser. Energy: The capacity for doing work (watts multiplied by seconds joules). Intensity: the power transmitted by a light wave across a unit area perpendicular to the wave. Power: the time rate of doing work (watt) Power density: the power of the laser beam per unit area (watts/cm2). Excitation: The addition of energy to a particle or system. Fiberoptics: a system of flexible quartz or glass fibers with internal reflective surfaces that pass light through thousands of glancing reflexes. Aiming beam: HeNe of low density beam used to guide the invisible laser light to the treatment area. Laser medium: (active medium) material used to emit the laser light. tem00: The lowest order mode possible , a gaussian or bell-shaped distribution of light intensity across the laser beam cross-section. tem:Transverse electromagnetic mode. Argon: gas used as a laser medium. Coagulation: destruction of tissues by heat without physically removing it. Vaporization: conversion of a solid or liquid into a vapor. Collimation: all rays coming from laser are parallel to each other. Coherent radiation:same wavelengths move together to different points. Thermal relaxation time: The time it takes heat to diffuse out of a structure and into surrounding structures by thermal conduction. When pulsed duration of a laser is shorter than the time required for heat to spread out of a target, the heat damage will be confined to the target. Target site: tissue that is aimed or fired with the laser beam. Gaussian curve: Normal statistical curve showing a peak with even distribution on either sides. Photocoagulation: tissue coagulation by laser light. Mode : the way in which laser beam is distributed.
|
| Contents | << Previous Chapter | Search |